A Plausible Link Between the Brain,
the Cervical Spine, and
Cerebral Spinal Fluid Flow
Front End Story
Jim McMahon was a great football quarterback. He was a two-time All-American at Brigham Young University. He was a first round National Football League (NFL) pick (number 5 overall). In the NFL he played for the Chicago Bears, San Diego Chargers, Philadelphia Eagles, Minnesota Vikings, Arizona Cardinals, Cleveland Browns, and Green Bay Packers, earning two Super Bowl Championships. He appeared on the cover of Sports Illustrated numerous times (1). During his playing career, McMahon suffered four documented concussions.
Sixteen years after he retired from football, at age 53, McMahon appeared on the cover of Sports Illustrated (September 10, 2012 issue) once again (2). It was an article detailing his struggles with dementia. Melissa Segura’s article is profiled:
NFL Concussions The Other Half Of the Story
THE WOMEN BEHIND THE MEN TOO OFTEN FORGOTTEN IN THE NFL CONCUSSION DEBATE ARE THE WIVES AND GIRLFRIENDS WHO BEAR
THE BURDEN OF CARING FOR SUFFERING PLAYERS—AND WATCHING THE MEN THEY LOVE SLOWLY SLIP AWAY
One of the many women caring for retired NFL players. Laurie Navon frequently has her picture taken with her boyfriend, Jim McMahon—in case he wakes up one day and no longer remembers her.
McMahon’s behaviors included:
- Lying on the bed watching the ceiling fan go round and round.
- Significant excessive sleeping, like “hibernating.”
- Not remembering where he wanted to go.
- Stumbling on furniture he felt had been rearranged (it had not).
- Being unable to find the bathroom.
- Not knowing where he was.
- A change in personality: no longer charismatic, sweet, confident, funny, or warm.
- Boarding the wrong airplane flight.
- He would drop to his knees, break into a cold sweat and turn a ghostly white, complaining of a pain that he compares to having an ice pick in his brain.
To compensate, his girlfriend:
- Printed a card with his vital statistics and her phone number and placed it in his wallet.
- Programmed their car’s GPS with their address and her phone number.
- Made sure the home alarm was on at all times in case he tried to wander off alone.
••••••••••
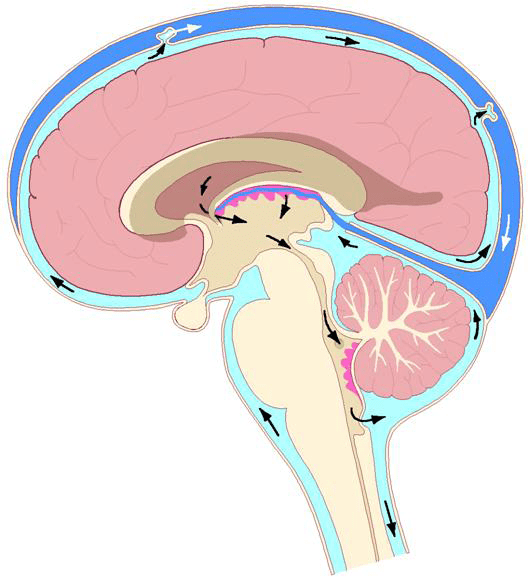
In most of the body there is a dynamic balance within the vascular system: the arteries carry blood (and all of its contents) to the tissues and to cells of the body, and the veins return the depleted blood back to the heart for replenishment and redeployment. The arteries and veins are functionally and physiologically linked. Any interruption of the artery-vein relationship is devastating for the involved tissues, and as such for the individual.
In the brain and spinal cord, the artery-vein relationship has a third player: the cerebral spinal fluid. It is the cerebral spinal fluid that is primarily responsible for maintaining the health of the neurons of the brain and spinal cord. However, because the cerebral spinal fluid is made in the brain from the brain’s blood supply, any compromise of either brain arterial supply or venous drainage will adversely affect the flow of cerebral spinal fluid.
Clinical assessment of upper cervical spine-brain biomechanics and physiology involve the utilization of special (upright weight bearing) MRIs and specific cervical spine radiographs. In 2003, Marshall Deltoff notes (3):
“Upper cervical practitioners utilize the radiographic measurement of static vertebral misalignment to help determine on which side and at what angle the adjustment [specific spinal manipulation] should be given.” p. 59
“MRI is an invaluable aid in diagnosing disorders of the brainstem, medulla, upper cervical cord an spinal canal. Congenital lesions, intramedullary and extramedullary intradural disease, including tumours, infection, ischaemia and demyelination can be assessed. MRI also provides valuable information about the encompassing bony and ligamentous structures of the cranio-vertebral junction and the cervical spine.” p. 57
••••••••••
In 2011, an important study appeared in the journal Physiological Chemistry and Physics and Medical NMR, and titled (4):
The Possible Role of Cranio-Cervical Trauma and Abnormal CSF Hydrodynamics in the Genesis of Multiple Sclerosis
In this study, eight multiple sclerosis (MS) patients and seven normal volunteers were MRI scanned with a quadrature head-neck combination coil to visualize the overall cerebral spinal fluid (CSF) flow pattern. The advent of phase coded MR imaging has made it possible to visualize and quantify the dynamic flow of CSF within the cranial vault and spinal canal. The findings were best visualized with an upright weight-bearing MRI. These authors note:
“Upright cerebrospinal fluid (CSF) cinematography and quantitative measurements of CSF velocity, CSF flow and CSF pressure gradients in the upright patient revealed that significant obstructions to CSF flow were present in all MS patients.”
Abnormal CSF flows were found in all eight MS patients. “The abnormal CSF flows corresponded with the cranio-cervical structural abnormalities found on the patients’ MR images.”
“Every MS patient exhibited obstructions to their CSF flow when examined by phase coded CSF cinematography in the upright position.”
“All MS patients exhibited CSF flow abnormalities that were manifest on MR cinematography as interruptions to flow or outright flow obstructions somewhere in the cervical spinal canal, depending on the location and extent of their cervical spine pathology. Normal examinees did not display these flow obstructions.”
“The abnormal CSF flow dynamics found in the MS patients of this study corresponded to the MR cervical pathology that was visualized.”
“The findings raise the possibility that interventions might be considered to restore normal intracranial CSF flow dynamics and intracranial pressure.”
“The findings further suggest that going forward, victims of Motor Vehicle Whiplash injuries with persisting symptoms, e.g., headache, neck pain, should be scanned by UPRIGHT(R) MRI to assure that their CSF hydrodynamics and cervical anatomy (C1- C7) are normal. Should their CSF hydrodynamics prove abnormal, they should be monitored by UPRIGHT(R) MRI to assure they are restoring to normal over time, or ultimately decompressed by expansion stenting or cervical realignment if they are not.”
This is an important article for chiropractors. These authors suggest that cervical spine malalignment obstructs the flow of cerebral spinal fluid. This obstruction of CSF flow increases intracranial pressure, leading to additional brain pathology and dysfunction.
These authors suggest that the improvement in cranial-cervical malalignment could improve cerebral spinal fluid flow, stopping the aforementioned cascade. In fact, in one of the MS patients, the UPRIGHT MRI found a malalignment of the occiput-C1. This malalignment was successfully treated by an upper cervical chiropractor. The authors noted:
“The patient’s symptoms, severe vertigo accompanied by vomiting when recumbent and stumbling from unequal leg length, ceased upon treatment.” Objective improvements in obstructed CSF fluid was also noted “immediately following treatment with the [chiropractic adjustment].”
••••••••••
In 2015, another important study appeared in the journal Neurology Research International, and titled (5):
The Role of the Cranio-cervical Junction in Cranio-Spinal Hydrodynamics and Neurodegenerative Conditions
The author notes that cranio-spinal hydrodynamics refers to the relationship between blood and cerebral spinal fluid (CSF) volume, pressure, and flow in the relatively closed confines of the compartments of the cranial vault and spinal canal. He notes that cranio-spinal hydrodynamics can be disrupted by a number of mechanical lesions (congenital, degenerative, an acquired) of the cranio-cervical junction, stating:
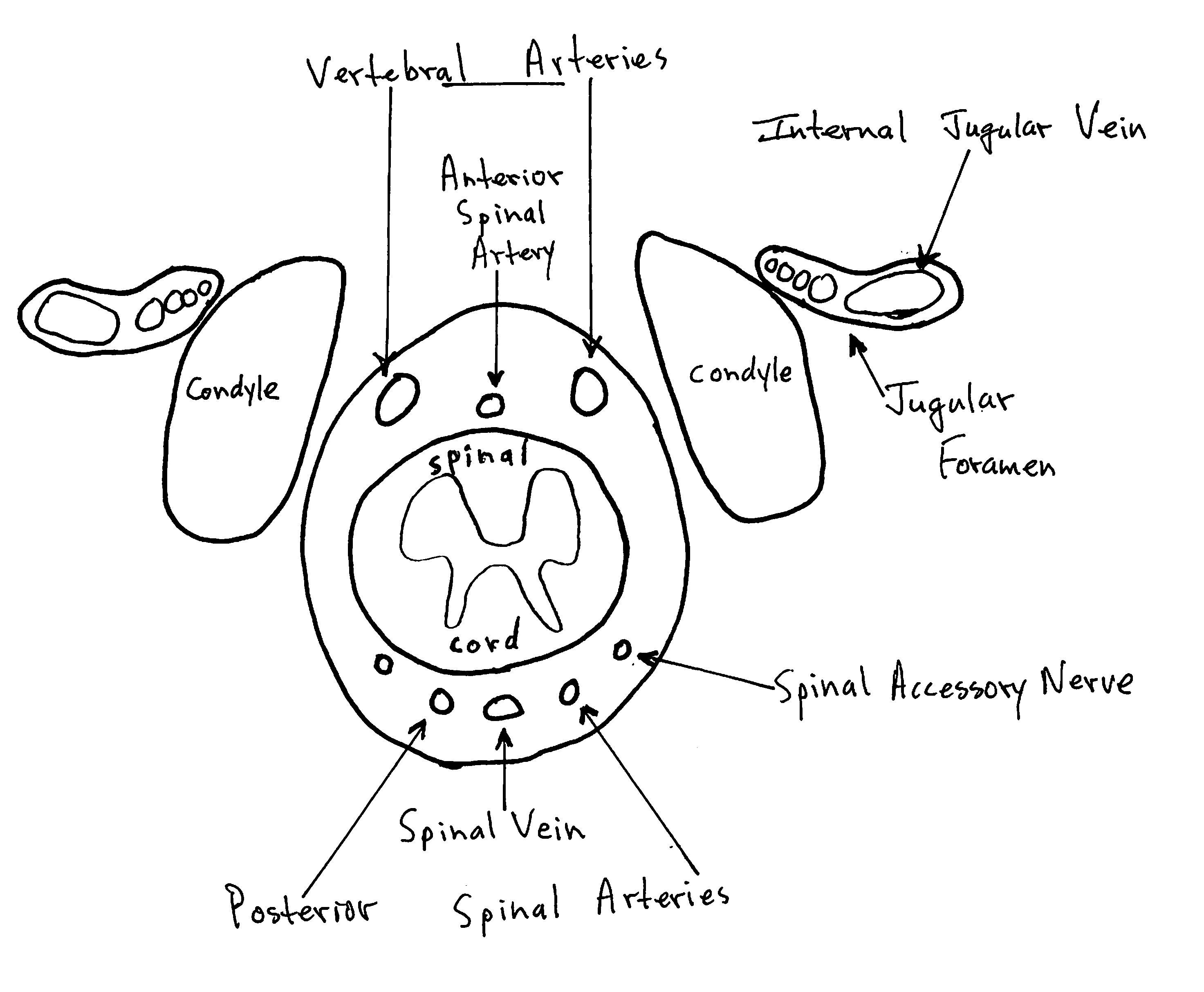
“The CCJ links the vascular and cerebrospinal fluid (CSF) systems in the cranial vault to those in the spinal canal.”
“The cranio-cervical junction (CCJ) is a potential choke point for cranio-spinal hydrodynamics and may play a causative or contributory role in the pathogenesis and progression of neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and ALS, as well as many other neurological conditions including hydrocephalus, idiopathic intracranial hypertension, migraines, seizures, silent-strokes, affective disorders, schizophrenia, and psychosis.”
“Malformations and misalignments of the CCJ cause deformation and obstruction of blood and CSF pathways and flow between the cranial vault and spinal canal that can result in faulty cranio-spinal hydrodynamics and subsequent neurological and neurodegenerative disorders.”
Congenital malformations/anomalies of the CCJ can block blood and CSF flow between the cranial vault and spine, pushing the cerebellar tonsils and/or brainstem into the cervical canal, which further blocks the flow of CSF. This causes an accumulation of fluid in the cranial vault (hydrocephalus). Such conditions include:
- Chiari malformations
- Abnormal clivoaxial angle (6)
- Hypoplasia of the posterior cranial fossa
- Basilar invagination
- Platybasia
- Hypoplasia of the foramen magnum
- Hypoplasia of the jugular foramen
- Anomalies of the odontoid process
- Premature closure of cranial sutures (craniosynostosis)
An acquired blockage to CSF flow, important to chiropractors, is a misalignment of the atlas on the occipital condyles. This author states:
“Misalignments of the CCJ [atlas-occiput articulation] can obstruct blood flow through the vertebral arteries and veins that can lead to chronic [brain/cranial] ischemia and edema.”
“Blockage of blood and CSF flow due to malformations and misalignments of the CCJ may play a role in chronic [brain/cranium] ischemia, edema, hydrocephalus, and ventriculomegaly [enlargement].”
“The CCJ is a potential choke point for blood and CSF flow between the cranial vault and spinal canal that can cause faulty cranio-spinal hydrodynamics and subsequent chronic ischemia, edema, and hydrocephalus.”
“Malformations and misalignments of the CCJ may play a role in chronic [brain/cranial] ischemia and edema, which may in turn lead to neurodegenerative processes and subsequent diseases.”
“Malformations, misalignments, and deformation of the CCJ compress the vertebral veins, which may affect CSF flow.” “An increase in CSF volume in the brain can compress veins and decrease drainage.”
This author emphasizes that the cranial-cervical junction is a choke point for cerebral spinal fluid flow between the cranial vault and spinal canal. He believes that manual, mechanical, and surgical correction of cranial-cervical junction structural problems will improve faulty cranio-spinal hydrodynamics and improve patient pathology and symptomatology, stating:
“Manual and surgical methods for correcting obstructions, as well as manipulation of blood and CSF flow, may help to restore or improve faulty cranio-spinal hydrodynamics in certain cases and decrease the prevalence, progression, and severity of neurodegenerative and other neurological conditions.”
A summary of his pathophysiological model is as follows:
- An increase in brain, blood, or cerebral spinal fluid volume in the cranial vault can cause compression of the bridging veins and lead to venous hypertension.
- Venous hypertension decreases cerebral arterial inflows.
- Chronic decreases in arterial flow can lead to oxidative stress, ischemia, and subsequent atrophy resulting in a compensatory increase in cerebral spinal fluid volume.
- Enlarged ventricles and cisterns are a sign of hydrocephalus and an increase in cerebral spinal fluid volume that can be caused by atrophy or chronic strains and deformation of the brain and brainstem.
Dr. Flanagan notes that the blockage of cerebral spinal fluid flow at the cranial-cervical junction may be predisposed by a combination of congenital and/or degenerative conditions. Small misalignments of cranial-cervical alignment, superimposed on such congenital and/or degenerative conditions, increase the likelihood of an obstruction of the cerebral spinal fluid flow. The author notes that manual therapy/manipulation of the upper cervical spine has the potential to improve the flow of cerebral spinal fluid, improving the patient’s signs and symptoms.
Axial View of the Foramen Magnum and its Contents, from below:
Back End Story
Recently (2016), Jim McMahon has appeared prominently again in the media. He has been profiled in an ESPN Special Report as a consequence of a change in his clinical status. The signs and symptoms of his chronic neurodegenerative disorder have quickly and dramatically improved, and consistent with his character, he’s talking about it (8).
An upright weight-bearing MRI was taken of McMahon’s head and neck. As noted above, the imaging showed an accumulation of fluid (cerebral spinal fluid) in his skull and around his brain. Consistent with the biomechanics and physiology reviewed in this article, McMahon’s upper cervical specific chiropractor took precise radiographs of McMahon’s upper neck and skull. A careful, precise, mathematical analysis of his radiographs showed that there was a meaningful malalignment between the skull and the atlas vertebra. Such findings are consistent with an impairment of fluid flow (venous, arterial, cerebral spinal) between the skull (brain) and the spinal canal. This biomechanical finding could account for the increased fluid noted in the MRI of his brain. The increased brain fluid could account for the plethora of signs and symptoms McMahon was suffering from.
Prior to this unique treatment, the ESPN Special noted that McMahon, age 56, was suffering from:
- Bad headaches
- “Pressure in my skull”
- Couldn’t see very well
- Couldn’t talk very well
- “All I wanted to do is lay down because my head was constantly pounding”
These findings and physiological explanations pertaining to Jim McMahon are plausible and have been supported by others. For example, in 2007, researchers from Rush University in Chicago noted (7):
“Unlike other vertebrae, which interlock one to the next, the Atlas relies solely upon soft tissue (muscles and ligaments) to maintain alignment [with the occiput]; therefore, the Atlas is uniquely vulnerable to displacement.”
“Displacement of C-1 is pain free and thus, remains undiagnosed and untreated, whereas health-related consequences are attributed to other etiologies.”
“Minor misalignment of the Atlas vertebra can potentially injure, impair, compress and/or compromise brainstem neural pathways.”
“Changes in the anatomical position of the Atlas vertebra [with respects to the occiput] and resultant changes in the circulation of the vertebral artery…”
“Anatomical
abnormalities of the cervical spine at the level of the Atlas
[-occiput] vertebra are associated with relative ischaemia of the
brainstem circulation.”
“Manual correction of this mal-alignment has been associated with reduced arterial pressure.”
Following the precise analysis of his upper cervical spine-occiput biomechanical relationships, Jim McMahon was carefully and specifically adjusted. The sole goal of the adjustment was to establish perfect alignment between the occiput and the atlas vertebrae. This goal was achieved, verified by post-adjustment radiographs that were similarly biomechanically analyzed. The improvement in his signs and symptoms were essentially instantaneous.
A post adjustment upright weight-bearing MRI of McMahon’s brain and spinal cord showed a remarkable reduction of fluid, as if an inverted bottle had been uncorked. McMahon’s improvement in clinical status is both substantial and appears to be long lasting. Within two minutes of the adjustive procedure, McMahon commented:
- “It was like the toilet flushed”
- “I could feel the stuff leaving my brain”
- “My eyes cleared up”
- “My speech cleared up”
A post treatment MRI showed significantly less fluid accumulation on McMahon’s brain. McMahon commented that the procedure “kept me from having bad pains and suicidal thoughts, and having me function fairly normally.”
Summary
This paper presents a plausible explanation as to the mechanism of how upper cervical-occiput misalignments might impair the venous, arterial, and cerebral fluid flows between the brain and spinal cord. It also suggests that a specific, precise, upper cervical chiropractic adjustment that results in improved alignment between the occiput an the atlas can “uncork” the flow of these fluids between the brain and spinal cord, resulting in an improvement of a plethora of clinical signs and symptoms.
REFERENCES
- Hendricks M; Super Bowl-winning quarterback Jim McMahon says he wishes he had played baseball; Yahoo September 27, 2012.
- Segura M; The Other Half Of the Story; THE WOMEN BEHIND THE MEN; Sports Illustrated; September 10, 2012.
- Deltoff MN; “Diagnostic Imaging of the Cranio-Cervical Region”, Chapter 4, in The Cranio-Cervical Syndrome, Mechaniscm, Assessment and Treatment; Edited by Howard Vernon; Butterworth Heinemann; 2003.
- Damadian RV, Chu D; The Possible Role of Cranio-Cervical Trauma and Abnormal CSF Hydrodynamics in the Genesis of Multiple Sclerosis; Physiological Chemistry and Physics and Medical NMR; September 20, 2011; 41; pp. 1–17.
- Flanagan MF; The Role of the Cranio-cervical Junction in Cranio-spinal Hydrodynamics and Neurodegenerative Conditions; Neurology Research International; November 30, 2015. [epub]
- Coban G, Coven I, Cifci BE, Yildirim E, Yazici AC, Horasanli B; The Importance of Craniovertebral and Cervicomedullary Angles in Cervicogenic Headache; Diagnostic and Interventional Radiology; March–April 2014; Vol. 20; pp. 172–177.
- Bakris G, Dickholtz M, Meyer PM, Kravitz G, Avery E, Miller M, Brown J, Woodfield C, Bell B; Atlas vertebra realignment and achievement of arterial pressure goal in hypertensive patients: a pilot study; Journal of Human Hypertension; May 2, 2007; Vol. 21; No. 5; pp. 347-357.
- https://www.youtube.com/watch?v=4ZxIUz4sc0U
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”
